Pavel Kolkhir
Nat Rev Dis Primers. 2022 Sep 15;8(1):61. doi: 10.1038/s41572-022-00389-z
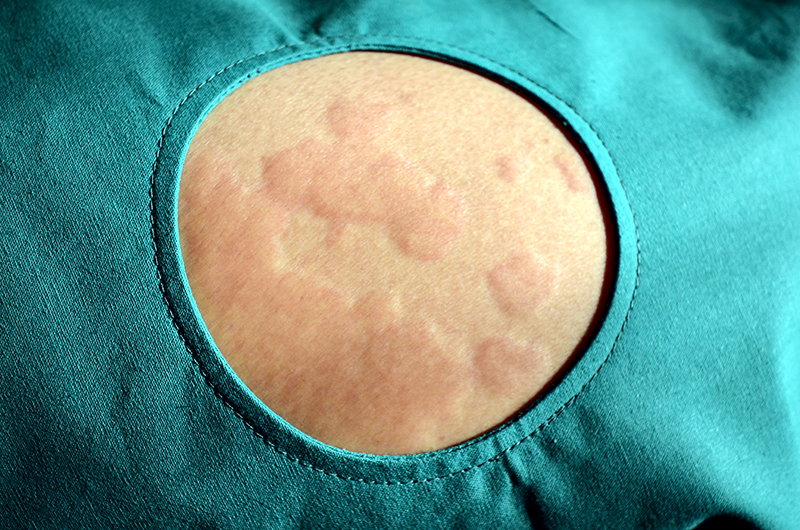
Urticaria is a common and heterogeneous inflammatory skin disease that affect up to 20% of the world population. Its symptoms include wheals, angioedema or both which are due to the stimulation and degranulation of skin mast cells and release of histamine and other mediators. Acute urticaria accounts for the majority of cases can last up to 6 weeks and be related to infections or intake of drugs or food. Chronic urticaria may be spontaneous or inducible, can last more than 6 weeks and persist for more than one year in most patients. Patients with chronic urticaria are deeply affected in their daily activities and may suffer from psychiatric comorbidities. Chronic inducible urticaria has different subtypes and triggers that lead to different symptoms.
The mechanism of chronic spontaneous urticaria includes autoantibodies, complement and coagulation cascades. Its diagnosis includes differential testing to identify underlying causes or triggers.
Urticaria treatment first line uses second-generation H1 antihistamines, and omalizumab and cyclosporine in a second line. Other new approaches focus on targeting mediators, signalling pathways and receptors of mast cells and other immune cells.
There’s still some research needed to define disease endotypes and their biomarkers, identifying new treatment targets and developing improved therapies.