Carvalho D, Aguiar P, Ferrinho P, Mendes-Bastos P, Palma-Carlos A.
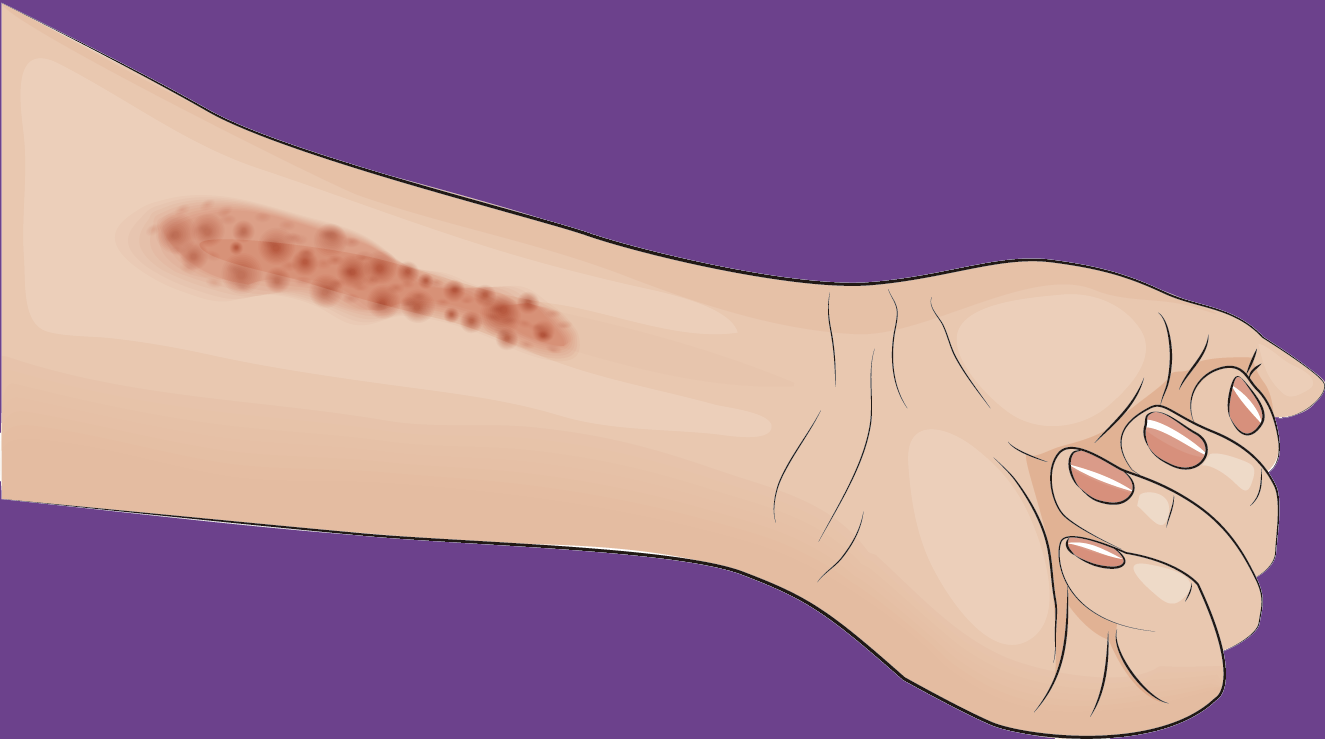
A prevalence study was conducted in Portugal to compare the rate of eczema and urticaria within regions and with other countries in Europe.
A telephone interview survey was performed in the last quarter of 2017. Investigators analysed 5000 phone calls to subjects over 16 years old, previously diagnosed with eczema or urticaria living in Portugal. The sample had a proportion representative by population, region, gender and age group.
They estimate the prevalence of eczema and urticaria in Portugal is 4,4 and 3,4%, respectively. Algarve is the region with the highest prevalence. Women are also more affected than men are and seem to be more at risk than men.
Overall, the prevalences found are higher than previously reported, but comparable to results from other countries. From a former study by Harrop and his team, in Europe atopic eczema is 0,14-0,60% of general eczema. Portuguese investigators estimate that atopic eczema prevalence in Portugal is around 0,61-2,64%.