Kaplan AP.
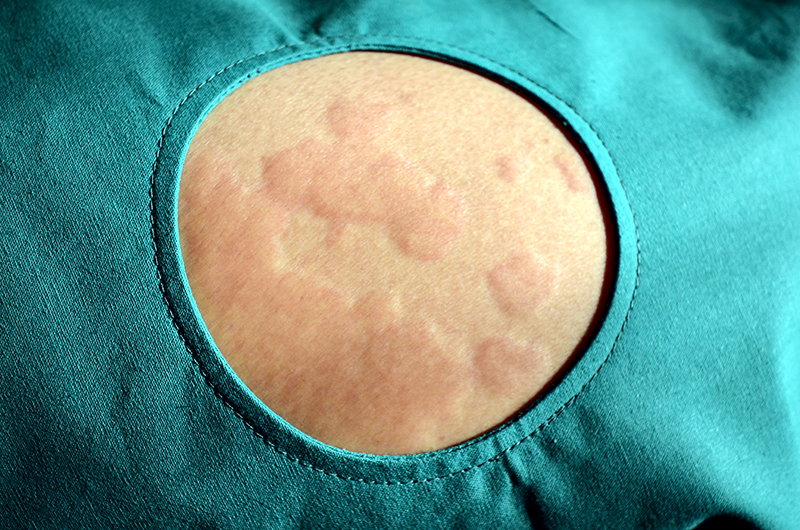
Urticaria can be divided into three general subtypes. Acute urticaria is defined as urticaria of relatively short duration that can be as brief as a day or two or can last up to 6 weeks. “Physical urticarias or inducible urticarias” consist of cold urticaria, cholinergic urticaria, and dermatographism as the most common, plus solar urticaria, local heat urticaria, aquagenic urticaria, vibratory urticaria/angioedema, and delayed pressure urticaria. The third subtype is chronic spontaneous urticaria (CSU) where the urticaria is present for over a minimum of 6 weeks up to many years.
Antihistamines are effective in about 50% of patients with CSU by interacting with the H1 receptor rendering it unresponsive to histamines. Omalizumab is effective in 65–80% of antihistamine-resistant patients and acts by binding IgE, thereby eliminating IgE directed to an autoantigen, downregulating IgE receptors, so that antireceptor antibodies are blocked, and ultimately leading to unresponsiveness of cutaneous mast cells and basophils. The addition of omalizumab represents a major advance because of its efficacy, easy utility, and favourable side-effect profile. Cyclosporine inhibits not only T cells but also histamine release from basophils and mast cells, has a success rate of about 70%, and is recommended third-line with care directed to potential side effects affecting blood pressure and renal function.
In conclusion, the use of antihistamines in high dosage (at least four times a day) is effective in close to half the patients with chronic spontaneous urticaria. For antihistamine resistance, the use of omalizumab has revolutionized therapy of antihistamine-resistant cases because of its efficacy and excellent side-effect profile. If the response is insufficient, cyclosporine is the next choice. Patients should be monitored regarding any adverse effects on blood pressure or renal function. All these are far safer than extended use of corticosteroid.