Prosty C, Gabrielli S, Ben-Shoshan M, Le M, Giménez-Arnau AM, Litvinov IV, Lefrançois P, Netchiporouk E
Front Med (Lausanne). 2022 Jul 7;9:926753. doi: 10.3389/fmed.2022.926753. eCollection 2022.
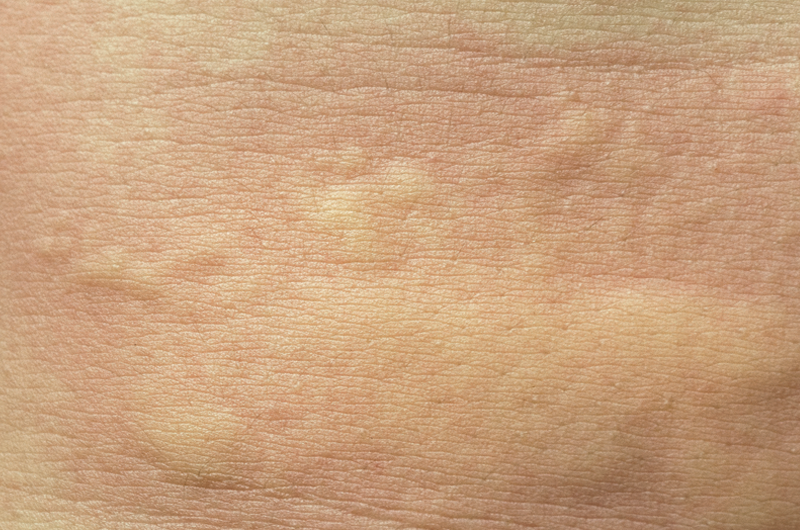
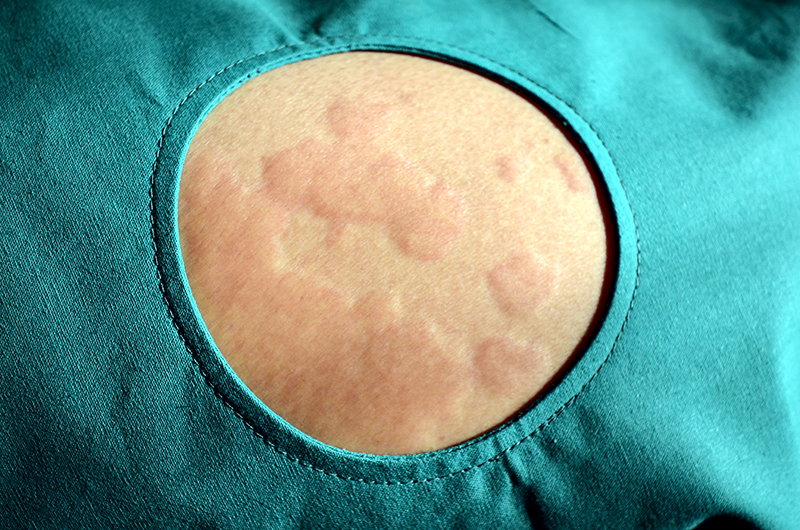
Chronic spontaneous urticaria (CSU) is defined by the presence of wheals and/or angioedema that occur in the absence of specific external stimuli and persist for more than 6 weeks. Its immunopathogenesis is not yet fully understood, but there are new trends on dividing patients into auto allergic and autoimmune subtypes.
The aim of this study was to investigate immune cells and pathways of CSU through the reanalysis of available transcriptomic data.
Investigators obtained microarray data of CSU and healthy control skin and blood from the Gene Expression Omnibus. Differentially expressed genes were analyzed using ToppGene and KEGG and cell-type enrichment was determined by CIBERSORT and xCell and correlated with clinical characteristics.
Th2 (IL-4/13 signaling) and Th17-related (IL-17/23 signaling) patways were found to be upregulated in lesional samples. CIBERSORT analysis showed that non-lesional samples had increased regulatory T-cells and resting mast cells. The xCell analysis revealed no significant differences between samples, however, Th2 scores in both types of samples correlated positively with disease severity. There were few differentially expressed genes and pathways identified between CSU and healthy control blood samples.
These results revealed and supported the connection of Th2 and Th17-related genes and pathways in CSU. Th2 scores related to disease severity, where increased resting mast cell and Treg scores in non-lesional samples indicate local suppression of wheal formation. Furthermore, disease activity seemed to be restricted to the skin as there were limited findings from blood. More studies are needed to further support this information.