Jorge Sánchez
J Allergy Clin Immunol Pract . 2020 Jul 14;S2213-2198(20)30700-5. doi: 10.1016/j.jaip.2020.06.057. Online ahead of print.
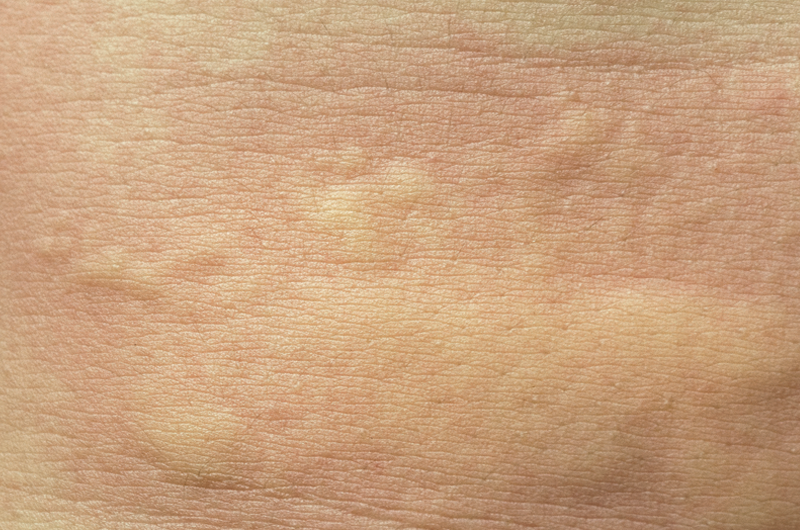
A great number of patients with chronic spontaneous urticaria experience exacerbations after treatment with non-steroidal anti-inflammatory drug (NSAID). Although international guidelines suggest that people with urticaria avoid NSAIDs, this is sometimes difficult. Some case reports recommend that H1-antihistamines can help prevent these exacerbations.
The objective of this study was to evaluate if H1-antihistamines can help prevent NSAID-exacerbated reactions in people with chronic spontaneous urticaria.
This was a cross-over, multi-center, and ambispective study in 3 centers in Medellín, Colombia that included 121 participants with chronic spontaneous urticaria and a history of NSAIDs exacerbations. A diagnostic challenge test without the use of antihistamines and a challenge test using antihistamines were performed using the NSAID reported in the medical record. The order in which test were performed in each participant was determined by the investigator: participants with a positive first diagnostic challenge, were subject to a second challenge using H1-antihistamines, those with a negative first challenge using H1-antihistamines, were subject to a second one without the use of H1-antihistamines, and those with a negative first diagnostic challenge or a positive first challenge using H1-antihistamines, did not undergo a second challenge. Some patients were subject to an alternative NSAID before the diagnostic challenge test or the challenge test using H1-antihistamines.
The diagnostic challenge test retrieved 96 participants testing positive, with 75 % (72 participants) tolerating the NSAID involved in the reaction when they added H1-antihistamines.
In conclusion, although NSAID may represent some restrictions for people with chronic spontaneous urticaria, the use of H1-antihistamines can help control further urticaria exacerbations due to NSAID treatment.