Gerasimos N. Konstantinou and George N. Konstantinou
(2019) Clin Transl Allergy
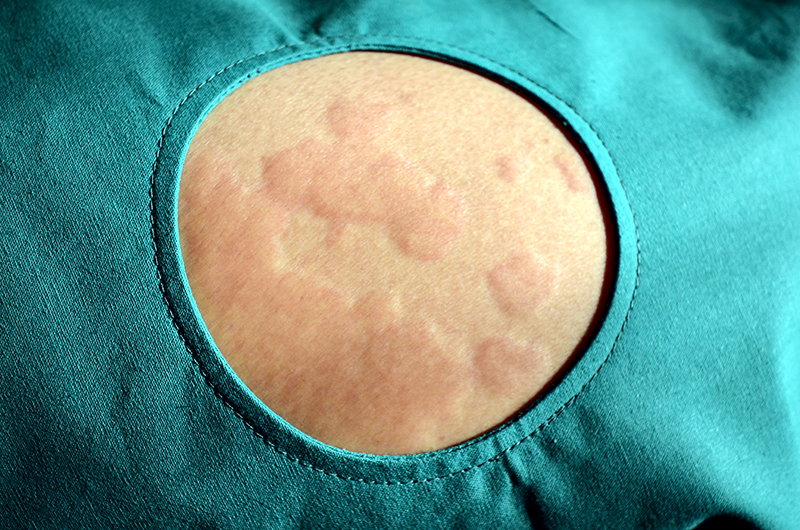
Chronic urticaria may affect the quality of life, namely in respect to an increase of psychiatric disorders.
This study aimed at evaluating the published evidence of psychiatric disorders that may coexist with chronic urticaria and the effect of psychiatric treatments on people with urticaria.
A systematic literature search for studies that investigated the existence of psychiatric comorbidity in patients with chronic urticaria was conducted, and twenty-five studies that met all the criteria were identified. Studies to be included in the study had to possess the following features: distinction between chronic urticaria and allergic conditions, direct collection of diagnostic psychiatric data by using clinical interview and standardized questionnaires, International Classification of Disorders criteria or the Diagnostic and Statistical Manual of Mental Disorders criteria for the diagnosis of mental disorders and manuscripts written or publish in English.
Analysis of the included studies showed that almost one out of three patients with chronic urticaria have at least one underlying psychiatric disorder. However, no studies clarified if the psychiatric disorder pre-existed at chronic urticaria onset and no association between chronic urticaria severity and duration and psychological functioning. Only a case report and two case series referred to the psychiatric disorder treatment as improving of urticaria.
This study shows the importance of a multidisciplinary approach involving recognition and management of any psychiatric disorder in addition to urticaria treatment.