Mohammed Elhendawy, Maha Hagras, Shaimaa Soliman, Engi Seif Shaker
Am J Clin Pathol. 2020 Sep 17;aqaa134. doi: 10.1093/ajcp/aqaa134. Online ahead of print.
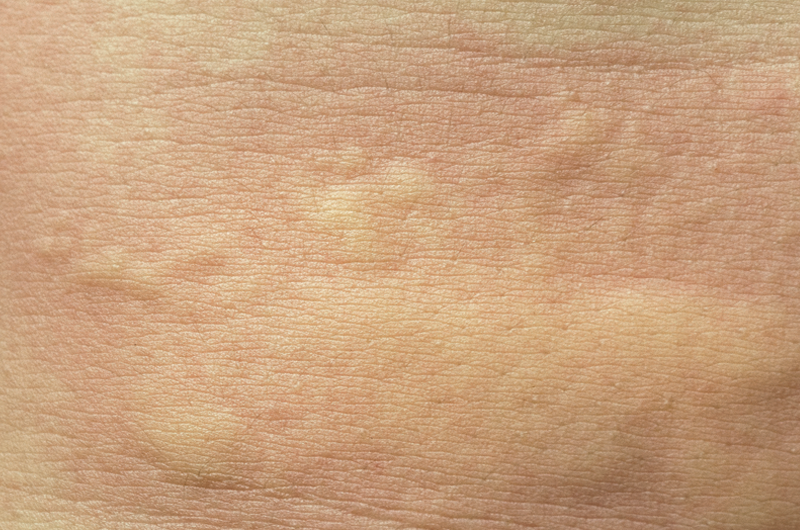
People with chronic urticaria have chronic hives, itching, and wheels that come and go for long periods. Chronic spontaneous urticaria represents 80 – 90 % of chronic urticaria cases, and the release of histamine and other inflammatory mediators from mast cells and basophils may be immunoglobulin E (IgE)–mediated or non-IgE-mediated. Helicobacter pylori is a gram-negative bacterium with a high prevalence worldwide, and that persistently colonizes the stomach. Its presence is associated with an increased risk of peptic ulcer and gastric cancer. The association between Helicobacter pylori and chronic spontaneous urticaria is controversial. This study’s objective was to assess the relationship between Helicobacter pylori eradication therapy and chronic spontaneous urticaria remission.
This was a randomized, double-blind, placebo-controlled pilot study that included 72 patients with urticaria. From these, 27 were positive for Helicobacter pylori stool antigen and PCR in gastric biopsy and were randomly assigned to receive anti-Helicobacter pylori treatment or placebo.
Participants with Helicobacter pylori had significantly lower hemoglobin concentrations with microcytic hypochromic anemia and a significantly higher occurrence of dyspepsia symptoms. All Helicobacter pylori patients (except 2) had significant improvement of the urticaria itching and red wheals after two weeks of therapy compared to placebo.
This study showed an association between chronic spontaneous urticaria and the presence of Helicobacter pylori in the gastric tissue. Patients with urticaria who do not respond to usual chronic urticaria treatment should be tested for Helicobacter pylori as therapy of Helicobacter pylori showed to improve the symptoms of chronic spontaneous urticaria.